COVID-19 patients are at significant risk for acute kidney injury (AKI). Studies have shown that patients hospitalized with the virus are twice as likely to develop AKI compared to non-hospitalized patients.
Here’s how COVID is affecting the kidneys:
- AKI is found in 24% to 57% of COVID hospitalizations and 61% to 78% of COVID ICU admissions.
- Of the COVID ICU patients with AKI, 35% required dialysis.
- Renal replacement therapy (RRT) is required in 5% to 39% of critically ill patients
- In an analysis of deceased COVID patients, 32% had kidney damage and 23% had AKI. In contrast, only 7% of hospitalized SARS patients had AKI.
Additionally:
- Patients who had not recovered kidney function at hospital discharge were less likely to achieve kidney recovery at outpatient follow-up.
- AKI caused by COVID-19 may cause a faster eGFR decrease after discharge. This occurred regardless of a patient’s comorbidities.
- COVID-associated AKI may progress to chronic kidney disease (CKD) because it may induce tubulointerstitial fibrosis.
The available evidence paints a picture that pathophysiology of COV-AKI is comparable to that of sepsis-associated AKI, which is caused by a multifactorial interplay of direct and indirect inflammation and cell death, framed by the concept that the clinical phenotype is predominantly the early expression of an adaptive response of the tubular cells to an injurious, inflammatory danger signal.”
The COVID Patient with AKI’s Journey
Patient
with AKI
catheter for
dialysis in groin
regular floor, gets
catheter in chest
for dialysis unit
treatment with
catheter in chest
used during
dialysis
with prolonged
catheter exposure
until an access is
placed
While some COVID patients with AKI heal, others do not and go on to need a fistula for dialysis. Because there’s no reliable way to determine if COVID patients with AKI will heal, many continue to use their catheters for dialysis in hopes that their kidneys will regain function.
How to Manage Acute Kidney Injury in COVID Patients
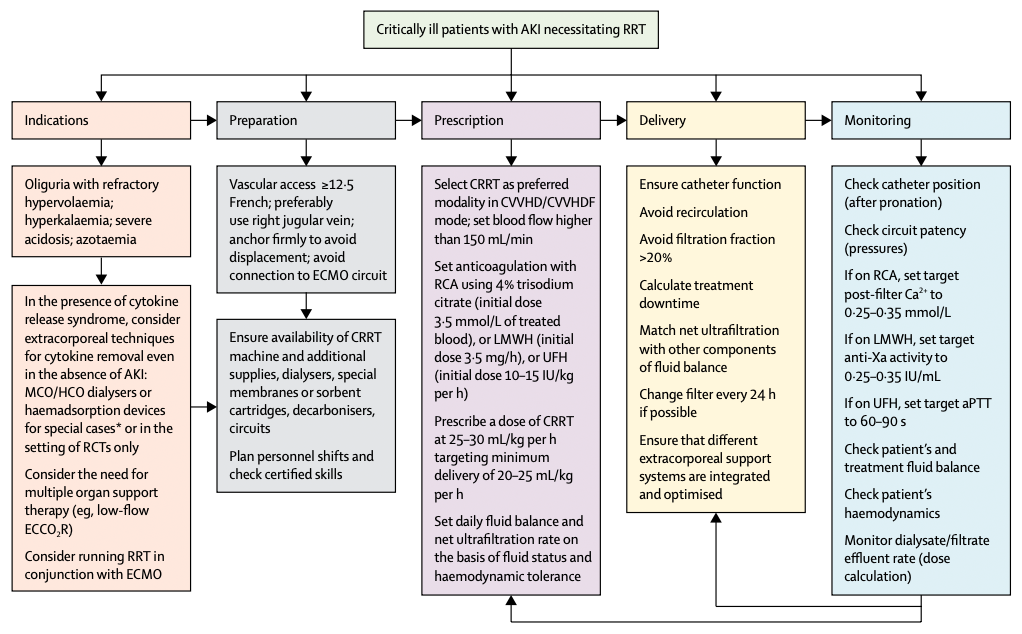
In the management of acute kidney injury in patients with COVID-19, Claudio Ronco, Thiago Reis, Faeq Husain-Syed, point out that:
- Kidney involvement in COVID-19 is common. Patients may initially present with protein in urine at hospital admission.
- Volume depletion could be a trigger for AKI.
- Lung-protective ventilation lowers the risk of AKI and helps prevent the worsening of the condition.
- Immune system dysregulation may be a factor in AKI.
- Early initiation of renal replacement therapy (RRT) and extracorporeal organ support (ECOS) prevent progression of disease severity and provide organ support.
Avoid Catheter Recirculation with Transonic Technology
Step 1:
MEASURE DELIVERED BLOOD FLOW RATE
With the bloodlines configured as normally used (document configuration), measure flow. Transonic Delivered blood Flow rate (Qb) is within 0-10% of the hemodialysis machine’s set blood pump speed or delivery flow rate.*
TRANSONIC DELIVERED BLOOD FLOW RATE (QB) IS WITHIN 0-10% OF HEMODIALYSIS MACHINE’S SET
Current blood pump setting is maximizing the Delivered blood Flow with the current catheter to bloodline configuration.
PROCEED TO RECIRCULATION MEASUREMENT
TRANSONIC DELIVERED BLOOD FLOW RATE (QB) IS >10% LOWER THAN THE HEMODIALYSIS MACHINE’S SETBLOOD PUMP SPEED OR DELIVERY FLOW READING*
Only proceed if both catheter lumens had blood return with treatment initiation. Using aseptic technique, reverse the catheter configuration by reversing the blood lines to the opposite lumens of the catheter than used for the initial measurement. Document configuration. Repeat the blood flow measurement.
TRANSONIC DELIVERED BLOOD FLOW RATE (QB) IS WITHIN 0-10% OF HEMODIALYSIS MACHINE’S SET OR DELIVERY FLOW READING*
Current blood pump setting is maximizing the Delivered Blood Flow with the current catheter to bloodline configuration.
PROCEED TO RECIRCULATION MEASUREMENT
TRANSONIC DELIVERED BLOOD FLOW RATE (QB) IS 10% LOWER THAN THE HEMODIALYSIS MACHINE’S SETBLOOD PUMP SPEED
Carefully document measurement and catheter configurations. Proceed to recirculation measurements with both catheter configurations. Escalate the results of the findings to the nephrologist for possible catheter evaluation or prescription adjustment to address catheter dysfunction.
*Some Hemodialysis Machine’s display both a Set Blood Pump Speed and Delivery Flow Reading. If both readings are displayed on your Hemodialysis machine use the Delivery Flow Reading
Catheter Configurations:
- Normal Configuration: Arterial Catheter Hub to Arterial Bloodline + Venous Catheter Hub to Venous Bloodline
- Reverse Configuration: Arterial Catheter Hub to Venous Bloodline + Venous Catheter Hub to Arterial Catheter Hub
Step 2:
CHECK RECIRCULATION
With the bloodlines configured from Step One with maximized Delivered Blood Flow Rate,
MEASURE RECIRCULATION: Recirculation is within 0 - 10%
RECIRCULATION IS WITHIN 0-10%
Current blood pump setting is maximizing Delivered Blood Flow with the current catheter to bloodline configuration.
RECIRCULATION IS GREATER THAN 10%
Only proceed if both catheter lumens had blood return with treatment initiation Using aseptic technique, reverse the catheter configuration by reversing blood lines to the opposite lumens of the catheter than used for the initial measuremen.
REPEAT RECIRCULATION MEASUREMENT
RECIRCULATION IS WITHIN 0-10%
Current blood pump setting is maximizing the Delivered Blood Flow with the current catheter to bloodline configuration.
RECIRCULATION IS GREATER THAN 10%
Carefully document measurement and catheter configurations. Escalate the results of the findings to the nephrologist for possible catheter evaluation or prescription adjustment to address catheter dysfunction.
How the Increase in COVID Patients who Need Dialysis is Affecting Clinics
Nephrology nurses have been in short supply for at least a decade. This is in part due to the specialized training a nephrology nurse needs to be and feel competent. However, with clinic patient volume potentially increasing due to COVID complications, and a significant portion of nurses nearing retirement, this shortage becomes an even bigger issue.
In dialysis clinics, it is estimated that there is a 5% to 7% shortage in nephrology nurses.
Retaining Nurses
High turnover among nephrology nurses is common due to the time it takes to become competent — 3 to 9 months. This is further threatened by a pandemic. Boyle SM, et al, recommend doing the following for retaining nephrology nurses:
Creating a Positive Work Environment: This includes creating a safe work environment — reducing exposure to hazards and minimizing physical demands, and prioritizing work-life balance.
Prioritizing Workplace Safety: Boyle SM, et al, report that the number of hours nephrology nurses work is a serious concern. Out of 1,070 nurses, 35% reported working over 12 hours per shift. These hours were higher among nurses providing inpatient dialysis. Organizations need to include nurse leaders in their executive committees to ensure policies prioritize workplace safety.
Offering Professional Development: Offer pathways for nurses to receive Certified Nephrology Nurse or Certified Dialysis Nurse. Nearly half of surveyed nurses reported their organizations did not offer professional development opportunities or reimbursement for those opportunities.
Recruiting Nurses
Many nursing schools have limited exposure to curricula on kidney replacement therapies. This can be remedied by partnering nurse leaders with nursing schools and through dialysis providers and organizations partnering with these schools.
Another way to increase recruitment is to utilize nurse residency programs. Offering loan forgiveness is another route to recruiting more nephrology nurses.
COVID-19 has created a dialysis crisis. Recruiting and retaining nephrology nurses and being aware of catheter recirculation and vascular access health, can help ensure better patient outcomes and a better work-life balance for nursing staff.

