For seven years since her kidneys totally failed, Mary Christiensen was driven three times each week to a clinic for hemodialysis. Even though this routine was draining, she stoically continued so she could feel better for a day or so after each treatment. It was only with her closest friends that she confided her underlying terror that, at any given moment, her vascular access, her link to successful dialysis, would fail, as it already had once. Mary was fortunate that time and another access was created for her to continue with the dialysis. Ultimately though, her access thrombosed and another access could not be created. She, as many others have, succumbed to end-stage renal failure.
Dialysis patients must plan their lives around their treatments, which often consume 20-28 hrs/week. This is time the patient can't spend with their family, at a job, or engaging in physical activity.
Treatment session times and transport (from cms.gov):
Time Needed for Hemodialysis
3 to 5-hour sessions, three times/ week, or 9-15 hrs/week
Median recovery time = 3 hours/ session, 9 hrs/ week
Transportation 2 - 4 hours.
TOTAL TIME/ WEEK = 20-28 hrs/week



Sources: Semin Dial. 2016 Sep; 29(5): 391–395, National Kidney Foundation
Francyne Rosenstock at Renal Reserve stated that the dialysis industry “for too long has treated people with kidney failure as unwitting victims, not educable consumers seeking the best treatment. And it's an attitude that encourages passivity and depression among the majority of its patients.” Finding ways to engage patients in their treatment plan and share control of the process can significantly improve their outlook.
Sources: WHO, National Kidney Foundation
Of the 2 million people who receive treatment for kidney failure, the majority are treated in only five countries – the United States, Japan, Germany, Brazil, and Italy. 80% of patients receiving treatment for kidney failure are in affluent countries with universal access to health care. Only 20% are treated in developing countries that make up the majority of the world population.
Compounding the problem is a global shortage of doctors and nurses trained in Nephrology. Even in the United States, with a sophisticated health care system, there is only one Nephrologist for every 40,000 people. The lack of necessary workforce has huge implications for individual patients and public health in general.
Considering the shortages of nephrologists and all health workforce related to nephrology, it can be concluded that in most parts of the world, people who need kidney care receive either suboptimal care or no kidney care at all.
- Osman et all

Sources: Kidney Int. Dec 2011;80(12):1258-1270.
Kidney Int Suppl Published Online 2018 Jan 19 doi: 10.1016/j.kisu.2017.10.009


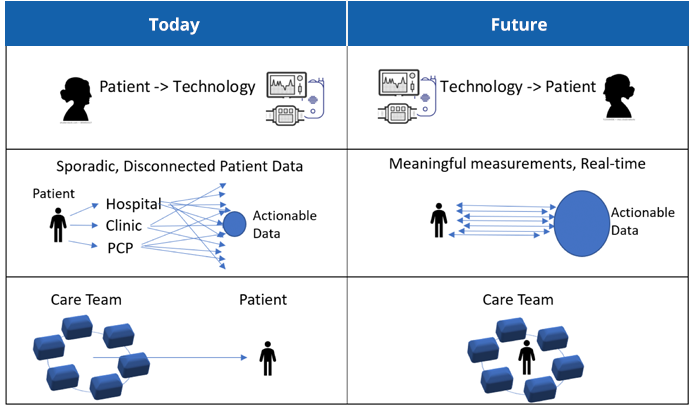
BENEFIT: more data for better informed decision making and early warning signs of potential issues and asynchronous events
BENEFIT: Improved mobility, portability, and potential for implantation

BENEFIT: Clinical decisions are supported with timely, actionable, trusted data, leading to less staff time and improved outcomes.
Predictive modeling can provide clinicians with additional insights into the risks and benefits of treating patients earlier, with the goal of reducing the number of Americans developing end-stage renal disease in the first place” says Lauren Neal, a principal at Booz Allen Hamilton.
This technology spotlight features 3 new solutions being developed which are poised to enable the paradigm shift from clinic management to home and ambulatory care.
Outset Medical, a medical technology pioneer in the dialysis field, is developing a suite of products which will serve as all-in-one home hemodialysis solutions designed to reduce the barriers that have previously limited the adoption of home treatment. The first generation product, Tablo, requires relatively minimal training, provides dialysis on-demand, and involves only 3 treatments per week. All this without the limitations and risks associated with travelling to and negotiating dialysis clinics.
The brilliance of Tablo is a unique combination of patient-friendly design and advanced technology. It takes the complexity out of home dialysis in a couple of critical ways:
Behind Tablo’s simple facade lies a sophisticated information system that automatically collects and trends treatment information, giving providers access to timely, actionable data.
Having already received FDA clearance for Tablo earlier this year, Outset now has it’s first at-home dialysis patient, fifty-seven-year-old Tracey Amadi, who has been on dialysis since 2008 and received a kidney transplant in 2013. She trained to use the system at Physicians Dialysis in Somerville, New Jersey with Dr. Sunit Kabaria, staff members, and her 21-year-old daughter. “I am thrilled to be using this amazing system at home,” said Ms. Amadi. “Tablo has been so easy to learn and use. It gives me a lot more control over my life and time, which saves my family and me many hours each week.”
What lies around the corner for Outset has the potential to be even more exciting. In 2019, Outset was awarded a KidneyX Redesign Dialysis Prize for a next-generation concept device that includes accurate volume removal based on factors more reliable than weight and achieves high fidelity vascular access evaluation. The concept incorporates Transit Time Ultrasound flow technology to measure a host of other potential features, including:
The aim is to provide an expanded tool kit of meaningful data to guide treatment decisions, empower and engage patients, and improve outcomes.


Wearable Artificial Organs, Inc (WAO) is a development-stage medical device company in the dialysis industry which was founded by world-renowned nephrologist Dr. Victor Gura. WAO is develolping a Wearable Artificial Kidney, dubbed WAK, which has been awarded an FDA fast-track through the Expedited Access Pathway program.
The WAK was designed to mimic the function of a normal kidney, working 24x7 to remove waste product while maintaining healthy fluid levels. Some of the key innovations which make this possible are:

Dr. Gura modeling an early prototype of the WAK
WOA’s vision is of a future where dialysis patients are no longer tetheres to cumbersome machines multiple times a week, and forced into restrictive diets with countless medications. Instead, all dialysis patients will have the option to choose a mobile dialysis solution that allows them a life similar to their lives before their ESRD diagnosis.
WAO is currently working to reduce the size of the WAK from about 11 lbs down to 2-lbs, allowing patients to hide it under their clothes as they go to work or enjoy their lifestyle activities.The device will need 2 more successful clinical trials to obtain market approval. The company believes WAK has the potential to provide superior clinical outcomes, a better quality of life for ESRD dialysis patients, and dramatic cost-savings.
The Kidney Project, spearheaded by Technical Director, Shuvo Roy, PhD at UCSF, and Medical Director, William Fissell, MD, at Vanderbilt University Medical Center is developing a surgically implantable, self-monitoring, and self-regulating bioartificial kidney to perform the filtration, fluid and electrolyte balancing, and other biological functions of the natural kidney.
About the size of a coffee cup, the device is powered by the body’s blood pressure without the need for external electrical connections, batteries or immunosuppressant drugs. After a single surgery to establish a permanent blood connection, the bioartificial kidney will process blood 24 hours a day, eliminating the need for hemodialysis and its inconveniences.
The Kidney Project team is leveraging recent developments in silicon nanotechnology, biocompatible materials, and tissue engineering to create an implantable device that continuously filters toxins from the blood while also providing the other biological functions of a healthy kidney. The device consists of:
Left: Technical Director: Shuvo Roy, PhD University of California, San Francisco
Right: Medical Director: William Fissell, MD Vanderbilt University Medical Center

Courtesy of Shuvo Roy, UCSF
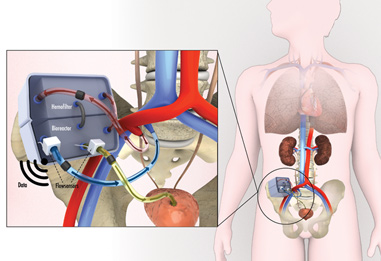
Incorporating physical and biochemical sensors, the device will be self-monitoring and self-regulating – that is, able to detect and monitor blood flow, urea clearance, and electrolyte balance. Information on device performance and the patient’s health status can be wirelessly sent to the provider. While still a few years away from commercial availability, The Kidney Project team believes this device can be an effective alternative to a kidney transplant, or dialysis, helping millions of ESRD patients to lead normal lives.
The technological advancements outlined in the previous chapter hold huge potential upside for patients with CKD:
From a population-based, disease management perspective, these technologies also offer significant potential for improvements in access, quality, and cost:
Ultimately, the most meaningful impact will be on patient quality of life. 84 year old Ward Shanahan, an CKD patient now on a home-based treatment, says it very simply:
I like to be able to get up in the morning, take a shower, and go around in the world. [This] gives me a life again.”
Sources: NPR, All Things Considered, 2019
© 2020 Transonic. All rights reserved. Privacy Policy